Esophagogastrodenoscopy
Esophagogastrodenoscopy
The best oncologist in Egypt, Dr. Ayman Abdel Hamid, consultant and teacher of advanced oncology and laparoscopic surgeries.
Continuing Education Activity :
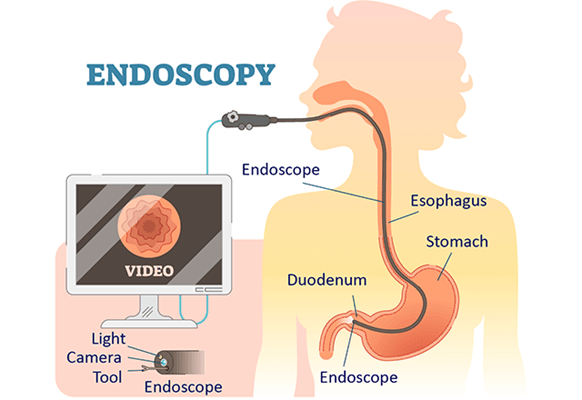
Esophagogastroduodenoscopy (EGD) is a diagnostic endoscopic procedure used to visualize the oropharynx, esophagus, stomach, and proximal duodenum.
It is one of the most common procedures for gastroenterologists.
This activity describes the diagnostic and therapeutic capabilities of upper endoscopy and highlights the role of the interprofessional team in looking after patients with pathology of the upper digestive tract.
Objectives :
Identify the indications for esophagogastroduodenoscopy.
Describe the technique for performing upper endoscopy.
Review the complications associated with esophagpgastroduodenoscopy.
Explain interprofessional team strategies for improving care coordination and communication to advance the appropriate and safe use of esophagogastroduodenoscopy to improve patient outcomes.
Introduction
Esophagogastroduodenoscopy (EGD) is a diagnostic endoscopic procedure that includes visualization of the oropharynx, esophagus, stomach, and proximal duodenum.
It is one of the most common procedures that a gastroenterologist performs.
Anatomy and Physiology
Esophagus
The esophagus is located posterior to the trachea and begins distal to the cricoid cartilage and ends at the cardiac orifice of the stomach.
It ranges in diameter from 4 to 6 mm and in length from 9 to 10 cm in the term infant to approximately 25 cm in the adult.
The change in the mucosa color from pale- to reddish-pink marks the transition from the esophagus and gastric epithelium (Z line).
Stomach
The stomach is usually located beneath the diaphragm and is approximately 40 cm distal to the incisors in an adult.
The area of the stomach where the esophagus enters is known as gastric cardia.
The portion of the stomach above the junction of the esophagus and stomach is known as fundus. It is visible in a retroflexed endoscopic view.
The majority of the stomach is known as stomach body.
Along the lesser curvature of the stomach is the incisura which divides the gastric body from the antrum. Endoscopically, the transition from the body to the antrum is from rugae to flat mucosa. The pylorus is the muscular opening between the lower end of the stomach and duodenum bulb.
Duodenum
The duodenum extends from the pylorus to the duodenojejunal angle.
The duodenum bulb is an expanded region immediately distal to the pylorus.
The duodenum then forms a C-shaped loop and endoscopically turns posteriorly and to the right for 2.5 cm, then inferiorly for 7.5 to 10 cm (descending portion), then anteriorly and to the left for approximately 2.5 cm, and finally connects to the jejunum at the level of ligament of Treitz.
Indications
Diagnostic
Persistent upper abdominal pain or pain associated with alarming symptoms such as weight loss or anorexia.
Dysphagia, odynophagia or feeding problems.
Intractable or chronic symptoms of GERD.
Unexplained irritability in a child.
Persistent vomiting of unknown etiology or hematemesis.
Iron deficiency anemia with presumed chronic blood loss when clinically an upper gastrointestinal (GI) source is suspected or when colonoscopy is normal.
Chronic diarrhea or malabsorption.
Assessment of acute injury after caustic ingestion.
Surveillance for malignancy in patients with premalignant conditions such as polyposis syndromes, previous caustic ingestion, or Barrett esophagus.
Therapeutic
Foreign body removal.
Dilation or stenting of strictures.
Esophageal variceal ligation.
Upper GI bleeding control.
Placement of feeding or draining tubes.
Management of achalasia (botulinum toxin or balloon dilation).
Contraindications
Absolute Contraindications
Perforated bowel.
Peritonitis.
Toxic megacolon in an unstable patient.
Relative Contraindications
Severe neutropenia.
Coagulopathy.
Severe thrombocytopenia or impaired platelet function.
Increased risk of perforation including connective tissue disorders, recent bowel surgery or bowel obstruction.
Aneurysm of the abdominal and iliac aorta.
Equipment
Gastroscopes
The standard gastroscopes have a diameter of 10 mm with an instrument channel of 2.8 mm. In children weighing less than 10 kg, endoscopes smaller than 6 mm in diameter for routine endoscopy should be used.
A gastroscope with a large operating channel measuring 3.8 to 4.2 mm is useful in severe acute upper GI bleeding.
High-definition gastroscopes with optical zoom should be available to screen for pre-malignant gastric or duodenal lesions.
Accessories
The biopsy forceps (standard and jumbo) are needed for tissue sampling. For retrieval of a foreign body during esophagogastroduodenoscopy (EGD), rat tooth forceps, alligator forceps, retrieval net, polypectomy snare, overtubes of esophageal and gastric lengths, and a foreign body protector hood should be available. Additional equipment may be required if therapeutic procedures are anticipated.
Preparation
Routine endoscopy in children and adults is usually performed in an outpatient setting using parenteral or general anesthesia.
Occasionally, endoscopy is necessary at the hospital bedside or in an operating room.
Diet :
Preparation for elective upper endoscopy procedure involves a period of fasting.
As per American Society for Anesthesiologists (ASA) guidelines, patients should fast a minimum of 2 hours after ingestion of clear liquids and 6 hours after ingestion of light meals.
In emergency situations or in conditions where gastric emptying is impaired, the potential for pulmonary aspiration of gastric contents must be considered to determine (1) level of sedation, (2) whether endotracheal intubation should be considered to protect the airway or (3) whether the procedure should be delayed.
Medications :
Most medications can be continued and are usually taken with a small sip of water before endoscopy, although diabetes medications need to be adjusted due to the period of fasting before the procedure.
American Society for Gastrointestinal Endoscopy (ASGE) guidelines should be followed for decisions regarding the management of anti-thrombotic agents or for the use of antibiotic prophylaxis in at-risk patients before the endoscopy.
Sedation and Monitoring
Sedation is used in most patients not only to minimize discomfort but also to provide amnesia for the procedure.
All patients undergoing upper endoscopy require pre-procedural evaluation to assess their risk for sedation and to manage potential problems related to pre-existing health conditions.
The choice of sedation varies from conscious sedation delivered by the proceduralist or monitored anesthesia care provided by an anesthesiologist, and preferences for one type of sedation over another are largely based on training and available local resources.
For routine upper endoscopy, many endoscopists utilize intravenous sedation using propofol.
For therapeutic endoscopic procedures such as foreign body removal or in patients in whom cooperation is not anticipated, including very young patients, general anesthesia may be required.
ASGE guidelines recommend routine monitoring of vital signs in addition to clinical observation for changes in cardiopulmonary status during all endoscopic procedures performed under sedation.
Informed consent
Patients, parents, or legal guardians should provide informed consents before the Esophagogastroduodenoscopy (EGD) and for the administration of sedation.
Technique or Treatment
Handling the Endoscope
The endoscope is mostly held in the left hand.
The control section of the endoscope should rest comfortably in the palm of the left hand.
The thumb controls up or down movement of the tip of the endoscope using a large wheel.
The index finger and, at times, the middle finger control the suction, air, and water valves.
The right hand is used to advance and withdraw the endoscope and its axial rotation.
The right hand is also used to insert instruments such as biopsy forceps, cytology brushes, needles for injection, hemostatic clips, polypectomy snares, foreign body retrieval instruments, and syringes for irrigation via the biopsy channel.
Esophageal Intubation
For esophagogastroduodenoscopy (EGD), patients are typically placed in left lateral decubitus with neck flexed forward.
A bite block is placed in the mouth before the endoscope is inserted into the oral cavity.
The endoscope is introduced into the mouth and to the base of the tongue under direct visualization.
The tip of the scope is then gently angulated downward until the vocal cords, epiglottis, both piriform sinuses, and cricoarytenoid cartilages are visualized.
The scope is then passed behind and to the right of the arytenoid cartilage towards the upper esophageal sphincter.
The upper esophageal sphincter is passed under direct visualization, often with application of gentle pressure while insufflating air.
Esophagus and Esophagogastric junction
After intubating the esophagus, the scope is advanced down the esophagus lumen while simultaneously examining the mucosa for any inflammation, ulcerations, furrowing, varices, narrowing or strictures.
The location of the esophagogastric junction should be noted.
The squamocolumnar junction, also referred as Z-line, is the area where the squamous epithelial lining of the esophagus (pale pink colored) meets the columnar lining mucosa of the stomach (salmon-colored).
The level of the Z-line should also be noted. If the Z-line is displaced proximal to the gastroesophageal junction, biopsies should be taken to evaluate for Barrett esophagus.
Stomach
The stomach is entered after passing the esophagogastric junction.
Once the stomach is entered, any residual gastric secretions should be suctioned, and air is insufflated to improve visualization.
The endoscope is then advanced while torquing to the right. The endoscope is advanced along the lesser curvature towards the pylorus, but to fill the greater curvature with the endoscope is usually necessary before the cannulation of the pyloric canal.
The pylorus is a small opening with radiating folds around it.
To pass through the pylorus, the endoscope is positioned in front of the pylorus, and a little air and gentle pressure should be applied against the orifice.
Duodenum
After passing through the pylorus, the endoscope enters the duodenum bulb.
The duodenum bulb should be examined on endoscope insertion rather than during withdrawal as passage of the instrument can cause possible mucosal changes.
After all four quadrants of the bulb are inspected the scope is advanced to the posterior aspect of the bulb; here the duodenum turns right sharply and takes downward turn.
To pass the superior flexure of the duodenum and enter the second part of the duodenum, the instrument is advanced using the dials and shaft torque, usually down and to the right followed by an upward spin of the dial.
The superior flexure of the duodenum is often passed blindly and examined on the way back.
The lower part of the second portion of the duodenum is reached by straightening the endoscope, in other words, pulling the endoscope slowly backward while maintaining the view of the lumen. This maneuver reduces the loop along the greater curvature of the stomach and, paradoxically, advances the endoscope into the distal duodenum.
The duodenum distal to the bulb has distinctive circular rings called valvulae conniventes.
The ampulla of Vater is found in the second portion of the duodenum and examined while withdrawing the endoscope.
After careful examination of the duodenum, pylorus, and antrum, the endoscope is retroflexed to visualize the gastric cardia and fundus.
The endoscope is then returned to a neutral position.
Once the stomach has been fully inspected, and biopsies, if necessary, are obtained, the endoscope is then withdrawn.
Before leaving the stomach, air should be suctioned.
The esophagus is again examined on withdrawal of the endoscope.
The average duration of a diagnostic EGD is 5 to 10 minutes under optimal sedation conditions.
Tissue sampling is obtained from suspicious lesions during EGD, although many gastroenterologists perform routine biopsies from designated sites, as a clinically significant disease may be present in an apparently normal looking mucosa.
Specimens obtained include biopsies, brushings of mucosal surface, and polypectomy.
Specimens are sent for histological, cytological, or microbiologic analysis based upon the type of the sample and clinical situation.
Complications
Complications following esophagogastroduodenoscopy (EGD) are rare, occurring in less than 2% of patients.
These could be related to sedation, endoscopy, and complications related to diagnostic or therapeutic maneuvers.
The most frequent and serious complications of sedation are cardiopulmonary.
Adverse events from over sedation include hypoxemia, hypoventilation, hypotension, airway obstruction, arrhythmias, and aspiration.
The complications following diagnostic EGD include infection, bleeding, duodenal hematoma, and bowel perforation.
The risk of bleeding following EGD with biopsy is 0.3%. Post mucosal biopsy bleeding can occur as intraluminal hemorrhage or intraluminal hematoma.
A duodenal hematoma is a rare complication of EGD with an unknown incidence and seems to occur more often in children than adults.
Bowel perforation occurs in less than 0.3 % of cases, and infection is rarely reported.
Complications typically are identified in the first 24 hours after the procedure.
Bleeding presents with hematemesis or bloody output from the gastrostomy tube.
Perforation is identified due to fever, tachycardia, abdominal pain or discomfort.
An abdominal x-ray should be done to reveal extra-luminal air.
Conservative therapy with bowel rest and antibiotics is the typical treatment, although some patients might require surgical repair.
Clinical Significance
Esophagogastroduodenoscopy (EGD) has become a key element in the diagnosis and treatment of esophageal, gastric, and small-bowel disorders.
The many accepted indications for EGD include evaluation of dysphagia, GI bleeding, peptic ulcer disease, medically refractory GERD, esophageal strictures, celiac disease, and unexplained diarrhea.
During EGD evaluation, diagnostic biopsies can be performed as well as therapies to achieve hemostasis and dilation for significant strictures.
If properly performed, it is generally a safe and well-tolerated procedure. EGD’s availability and use in the pediatric population have increased.
Decisions surrounding the conditions and time for EGD use in children remain more of an art than a science, and additional critical review of this tool’s use is needed to maximize results and minimize risk.
Enhancing Healthcare Team Outcomes
In the pediatric population, endoscopy is typically performed by a pediatric endoscopist with the medical knowledge and technical competency specific to perform safe and effective GI procedures in this population.
The American Society for Gastrointestinal Endoscopy (ASGE) published practice modification guidelines to provide guidance regarding performing endoscopy in infants and children.
If it is not possible for a pediatric-trained endoscopist to perform the procedure, an adult-trained endoscopist should perform endoscopic procedures in children in coordination with a pediatrician and pediatric specialists.
During endoscopic procedures, procedural and resuscitative equipment appropriate for pediatric use should be readily available.
If sedation is needed for the procedure, personnel trained specifically in pediatric life support and airway management should also be readily available.
In symptomatic children with known or suspected caustic ingestion, endoscopy should be performed within 24 hours.
It is recommended to perform emergent foreign body removal of esophageal button batteries as well as two or more rare-earth neodymium magnets.
Dr. Ayman Abdel Hameed :
The official page: Prof. Dr. Ayman Abdel Hameed, consultant and teacher of oncology surgeries and limited surgical intervention.
Doctorate in Oncology Surgery at the National Cancer Institute, Cairo University.
Master of Surgery oncology at the National Cancer Institute, Cairo University.
Bachelor of Medicine and Surgery, Faculty of Medicine, Kasr Al-Ainy, Cairo University, 2010, with distinction and honors.
More than 14 years of practical experience in surgery, oncology, and limited surgical intervention using surgical laparoscopes and surgical robots.
Book now : 01557112376
